Penicillin, Syphilis, and Drug Shortages

I recently visited the Alexander Fleming museum at St. Mary’s Hospital, London, together with my friend and fellow pathologist Dr. Suzanne Dintzis. It’s a tiny museum, maybe 20 square meters in all, consisting mainly of Fleming’s original laboratory where he discovered penicillin. Suzy and I had fun looking through the steam baths and incubators and various other microbiology lab instruments from almost a century ago.
Fleming is justifiably famous for his 1928 discovery involving an accidentally contaminated culture plate, but it wasn’t initially clear that it was going to be useful. The main problem was that neither Fleming nor any of the colleagues he spoke with could see a way to extract the drug from fungal cultures. And so penicillin was shelved for almost a decade. It wasn’t until 1937 that Howard Florey at Oxford stumbled across Fleming’s work, saw the potential, and picked up the baton. Three years later his team had managed to extract enough penicillin for a small pilot study in mice, and later in a human patient.
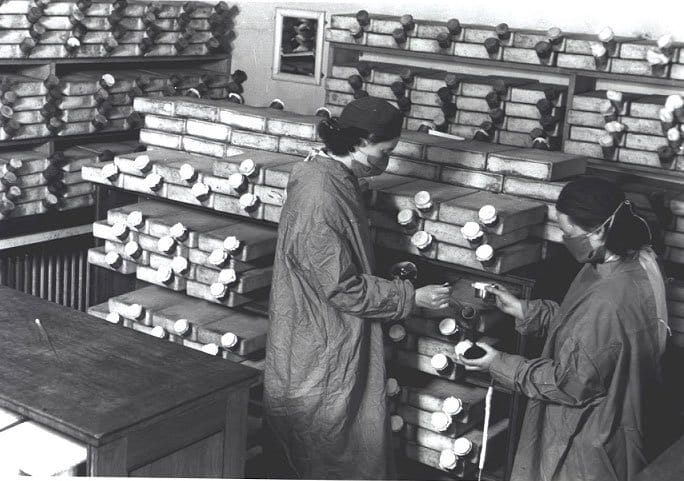
But many more problems needed to be solved before penicillin production could be scaled sufficient for use in medical practice. The photo below from the London Science Museum shows a room full of fermentation vessels at Oxford, staffed by six women who laboriously extracted a few milligrams of penicillin per week. It was only enough for a very small number of patients. Nurses were even collecting patients’ urine to recycle the drug for use in other patients. What was needed was industrial-scale manufacturing.
Because it was now 1941, and Britain’s manufacturing sector was fully focused on the war with Germany, Florey travelled to the US where he helped set up a penicillin program in a US Department of Agriculture lab in Peoria. There they developed and improved on techniques to ferment the yeast in much larger tanks, using improved strains of the fungus (one strain was discovered on a rotting melon in an Illinois market) as well as new growth media.
Having worked out key details of large-scale fermentation, the next logical step was to turn penicillin production over to the pharmaceutical industry. Initially, major pharmas were reluctant to commit, but once the US entered WWII, the market size for the product became clear. A number of manufacturers led by Pfizer built new production plants within a short period of time (4 months according to Pfizer’s website) and begin supplying penicillin for the war effort.
Fast forward to today. While many other antibiotics have been developed since then, penicillin remains a first-line therapy for several infections, notably syphilis. One injectable form, benzathine benzylpenicillin G, commonly referred to as PenG or by the trade name Bicillin, is the only safe and effective therapy for syphilis during pregnancy. We tend to think of syphilis as a historic disease, and it certainly was important historically. (Side note: another London museum, the Hunterian Museum located in the Royal College of Surgeons building, includes a number of skulls and other pathologic specimens showing the devastation of syphilis. Below is a photo I took on a recent visit.)

But syphilis is on the rise again, both in the US and globally. One explanation is that the COVID epidemic reduced screening for sexually transmitted infections. A particularly worrisome statistic is that there were almost 4000 cases of congenital syphilis reported in the US in 2022, a ten-fold increase from a decade earlier.
Which brings us to a big problem. In recent decades PenG has suffered from recurring shortages, and clinics often struggle to find enough doses to treat pregnant women. Why on earth is Pfizer, who was so proud of their ability to rapidly build factories to supply the troops during World War II, now struggling so much to keep up with demand? You won’t be surprised to hear that it’s complicated, that there’s plenty of blame to go around. The full story can be found in this excellent ProPublica piece.
It turns out that Pfizer has a monopoly on PenG within the US. Twenty years ago there were two other manufacturers, but Pfizer purchased both of them. Having one manufacturer rather than three greatly increases the risk of shortages due to manufacturing problems. And although it’s possible to import the drug from other countries, including France, the import prices are high (roughly $500/dose). Pfizer’s list price is also around $500/dose, though Pfizer is required by law to provide the drug for mere pennies per dose through Medicaid programs. Which raises an interesting question: if the overall profit margin were higher, would that attract new manufacturers to enter the market? Maybe, but it’s hard to know what that threshold is, esp. given the high startup and regulatory costs of running a pharmaceutical manufacturer. Any new market entrant would need some form of guaranteed volumes at an acceptable price in order to justify the investment.
So what can be done at this stage? My opinion is that the healthcare industry needs to take some supply chain lessons from Toyota. The key principles are described in this Harvard Business Review article.
Principle #1: Dual sourcing of most parts. Unlike other manufacturers, Toyota doesn’t do this mainly to play suppliers off against each other for low pricing. Rather, Toyota uses dual sourcing primarily for redundancy. From what I’ve read in other publications, Toyota guarantees each supplier enough purchase volume to maintain a strong incentive for each supplier to stay in the market for each supplied part.
Principle #2: Transparency. Toyota has famously close relationships with its suppliers, so much so that their in-house engineers and those of the suppliers will actively collaborate on designs. This arrangement also provides transparency such that if a supplier has any problems producing their product (for example, if one of the supplier’s suppliers is struggling) Toyota will know about it right away and will work with them on solutions. Pfizer, in contrast, has provided very little information to the FDA, let alone health systems and clinics, regarding its volumes and projections, according to ProPublica’s sources. (Pfizer, not surprisingly, begs to differ.)
Principle #3: Inventory management. Toyota is also famous for its just-in-time (JIT) supply chain processes, but even Toyota recognises that JIT supply chains have hitches from time to time. Toyota therefore monitors the the frequency of supply disruptions, and uses this information to continually adjust the size of the extra inventory for each part. For example, factories in some locations increase inventories of certain parts during winter months, when storms can delay deliveries with little advance notice.
The ProPublica piece cites two other proposed solutions to the problem of generic drug shortages, namely federal government manufacturing and stockpiling of key public health drugs such as PenG. And maybe these are good ideas. But I’d first like to see the pharma supply chain industry, including distributors and GPOs, get their collective acts together and start managing their pharmaceutical supply chains Toyota-style.
